Our Location
304 North Cardinal St.
Dorchester Center, MA 02124
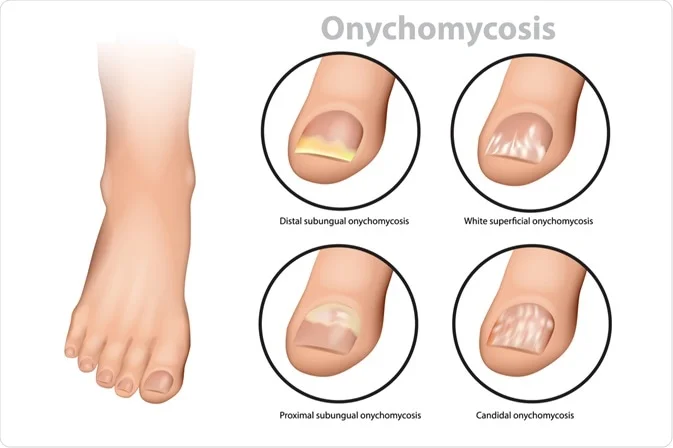
After treating thousands of patients with nail fungus over my years in practice, I’ve witnessed the frustration, embarrassment, and physical discomfort this condition causes. Today, I want to share the medical reality of onychomycosis and why understanding this condition is crucial for effective treatment.
As a medical professional, I can tell you that nail fungus, or onychomycosis, is far more complex than most people realize. It’s not simply a cosmetic issue or poor hygiene problem – it’s a legitimate medical condition caused by pathogenic fungi that have evolved specifically to thrive in keratin-rich environments like your nails.
The condition affects approximately 10% of the global population, with prevalence increasing dramatically with age. By age 70, nearly 50% of people will experience some form of nail fungus. This isn’t due to poor personal care – it’s a natural consequence of aging, reduced immunity, and cumulative exposure to fungal pathogens.
In my practice, I’ve identified three main categories of organisms responsible for nail infections:
Dermatophytes account for about 80% of toenail infections and 50% of fingernail infections. These organisms have evolved specifically to digest keratin, making them perfectly adapted to nail environments. Trichophyton rubrum is the most common culprit I encounter.
Yeasts, particularly Candida species, cause about 10% of nail infections, more commonly affecting fingernails. These infections often occur in people with compromised immune systems or those frequently exposed to moisture.
Non-dermatophyte molds make up the remaining infections and are increasingly common in certain geographic regions. These can be particularly challenging to treat with traditional antifungal medications.
Understanding how nail fungus develops is crucial for effective treatment. The process begins when fungal spores encounter microscopic breaks in the nail or surrounding skin. These entry points can be so small they’re invisible to the naked eye – created by minor trauma, aggressive nail trimming, or even wearing tight shoes.
Once inside, fungi begin colonizing the nail bed and nail plate. They secrete keratinase enzymes that break down keratin, literally eating away at your nail structure. This process creates the characteristic changes we see: thickening, discoloration, and brittleness.
The fungi also create biofilms – protective matrices that shield them from both immune responses and antifungal treatments. This is why nail fungus is so persistent and why simple topical treatments often fail.
In my years of practice, I’ve seen patients spend thousands of dollars on hospital-based treatments with mixed results. Traditional medical approaches include:
Oral Antifungal Medications cost $200-500 per treatment course, require liver function monitoring (additional $100-200 per test), and have success rates of only 60-80%. The medications also carry risks of liver toxicity and drug interactions.
Prescription Topical Treatments like ciclopirox lacquer can cost $300-600 for a treatment course and require daily application for up to a year. Success rates are even lower, around 35-55%.
Laser Therapy in clinical settings costs $500-1500 per session, with most patients requiring 3-6 sessions. Results are inconsistent, and insurance rarely covers the treatment.
Surgical Nail Removal is the most expensive option at $1000-3000, requires recovery time, and doesn’t guarantee the new nail will grow back fungus-free.
One of the most exciting developments in nail fungus treatment is photodynamic therapy and light-based treatments. This technology, once available only in expensive clinical settings, represents a breakthrough in home treatment options.
Light therapy works by targeting fungal cells with specific wavelengths that disrupt their cellular processes. Unlike chemical treatments that must penetrate the nail barrier, light energy can pass through nail tissue and directly affect fungal organisms beneath.
The science behind light therapy is compelling. Certain wavelengths of light generate reactive oxygen species within fungal cells, leading to cellular damage and death. Other wavelengths can heat fungal organisms to lethal temperatures while leaving surrounding healthy tissue unharmed.
The medical field is increasingly recognizing that effective nail fungus treatment doesn’t require expensive hospital visits or risky medications. Home-based light therapy devices represent a paradigm shift in how we approach onychomycosis treatment.
Cost Effectiveness: A one-time investment in a quality light device can provide unlimited treatments, eliminating the recurring costs of medications and clinical visits.
Safety Profile: Light therapy has minimal side effects compared to oral antifungals, making it suitable for patients who can’t tolerate systemic medications.
Convenience: Home treatment eliminates travel time, appointment scheduling, and the embarrassment some patients feel about their condition.
Consistency: Daily home treatment is easier to maintain than frequent clinical visits, improving treatment compliance and outcomes.
Recent studies have shown promising results for light-based nail fungus treatments. Research indicates that specific wavelengths can achieve fungal clearance rates comparable to or better than traditional treatments, with significantly fewer side effects.
In my clinical observations, patients using appropriate light therapy devices at home often show improvement within 4-6 weeks, with continued progress over 3-6 months of consistent use.
Regardless of the treatment method chosen, early intervention is crucial. I always tell my patients that nail fungus becomes exponentially more difficult to treat as it progresses. What might require a few weeks of light therapy in early stages could require months of treatment for advanced infections.
Don’t wait for the infection to spread to multiple nails or cause significant nail damage. The sooner you begin effective treatment, the better your outcomes will be.
While home treatment with light devices offers many advantages, it’s important to approach it scientifically. Proper diagnosis is still essential – not all nail changes are due to fungus, and treating the wrong condition will lead to frustration and wasted time.
If you’re considering home light therapy, ensure you’re using a device designed specifically for nail fungus treatment with appropriate wavelengths and safety features. Quality devices should provide clear usage instructions and realistic timelines for improvement.
Nail fungus is a legitimate medical condition that deserves effective treatment. The days of accepting expensive, risky, or ineffective treatments are behind us. With advances in light therapy technology, safe and effective home treatment is now a reality.
As a medical professional, I’m excited about the potential for patients to take control of their nail health without the barriers of cost, inconvenience, and side effects associated with traditional treatments. The future of nail fungus treatment is bright – literally and figuratively.
Remember, successful treatment requires consistency, patience, and the right approach. With proper home light therapy, you can achieve the healthy, clear nails you deserve without the expense and hassle of traditional medical treatments.